Lung cancer is a killer. It ends the life of more Americans than any other cancer. Frustratingly for those of us surgeons who do or have treated afflicted patients, the likelihood of developing lung cancer can be significantly diminished. Actively smoking or being exposed passively to the exhaled smoke from others is responsible for at least 80% of these lethal malignancies; avoiding these behaviors nearly eliminates the chance of having this diagnosis.
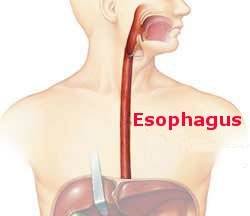
Second best to never having lung cancer is detecting it at an early stage, i.e., before it has spread to other organs or even to lymph nodes near the esophagus. If a lung cancer is confined within a lung and a full evaluation with the proper battery of tests show no spread the cancer is deemed to be in Stage I. Under these conditions, assuming the patient is in reasonable health otherwise, a surgeon can remove the involved part of the lung—usually a lobe but occasionally an entire lung—and give the patient a 70% to 80% chance of a cure. Once spread has occurred and there are metastases the likelihood of cure are low.
Clearly it is in a current or recent smoker’s best interest to do all they can to enhance the odds a cancer is detected at this early stage. Current screening techniques accomplish this. Chest x-rays are useful for screening but much better results are obtained with low-dose (of radiation) CT scans. Several reported studies with large numbers of patients show that screening—followed by appropriate treatment if a cancer is found—significantly lowers the likelihood of dying from lung cancer by 15% to 30%. These studies show that only a modest number of actual lives are saved; but, it matters a lot if your life is one that is spared. There are only occasional false positive scans.
Who should be screened? The criteria are in flux but as of now include the following: people who have a history of heavy smoking and smoke now or quit within the last 15 years and whose age is between 55 and 80 years.