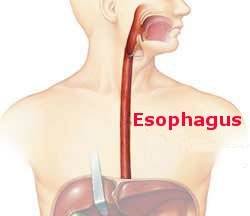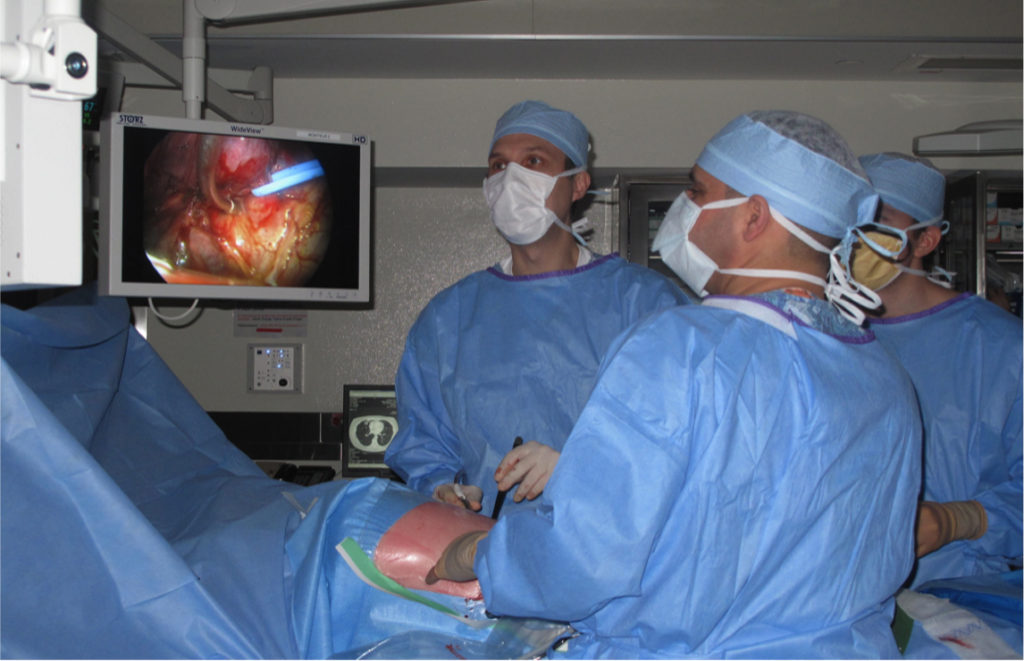
There are multiple considerations inside his or her head when a thoracic surgeon operates on a patient with lung cancer. I want to focus on two of them: how will the surgeon perform the operation and what part—how much—of the lung will the surgeon remove? A surgeon can gain access to and operate on the lung through a thoracotomy where the ribs are spread apart—the open approach—or use a minimally invasive technique with small incisions and a video camera for visualization. Once inside the chest when faced with lung cancer the surgeon can remove all of a lung (pneumonectomy), a lobe (lobectomy), a segment of a lobe (segmentectomy), or a pie-shaped wedge of lung (wedge resection). As the operative options scale from most to least amount of lung removed the impact on the patient’s breathing capacity also goes from most to least.
There are two absolute goals. First, the only reason to operate is to cure the cancer which means the thoracic surgeon must remove all of it; if “just a little” is left behind the cancer will recur and the procedure was for naught. Secondly, the patient must not only survive the operation but must not have their quality of life limited by breathlessness because the surgeon removed so much lung that the patient suffers significant lifestyle impairment afterwards as shortness of breath severely limits activities.
I won’t elaborate on how these two considerations are addressed; surgeons use many tests and their own judgement based on personal experience. As a minimum we can identify the priority of these goals for any operation for lung cancer: cure and maximum quality of life.