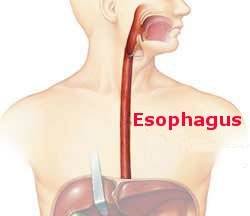
It seems time to revisit this topic. Barrett’s esophagus picked up its name years ago when the surgeon Norman Barrett in England performed an esophagectomy on a patient with an ulcer in the esophagus. The final pathologic exam of the esophagus showed that the cells lining the inside of the esophagus were not of the normal squamous type, resembling the cells of our skin, but were columnar in shape, like the cell that line the stomach and intestine. From this experience an eponym was born.
The condition Barrett described with an ulcer in the esophagus is rarely if ever seen now and the definition of Barrett’s esophagus is a moving target. The essential feature is the presence of this “inappropriate” columnar epithelium in the esophagus. The importance of this abnormality is that in some cases it is a precursor to the development of esophageal cancer so diagnosis and treatment are important.
Diagnosis requires an endoscopy and biopsy of the epithelium. Since most, perhaps all, patients have symptomatic GERD manifested with heartburn, endoscopy is appropriate for all those reflux sufferers whose symptoms are bothersome enough to seek medical attention.
Treatment depends on the findings. If a cancer is identified patients are treated with treatment being based on the stage of the malignancy. If the cells exhibit dysplasia, the columnar cells are abnormal but not cancerous, the epithelium is excised endoscopically or ablated with a laser. Finally if the cell are normal then follow-up endoscopy every few years is recommended so any tendency to develop a cancer can be detected at an early stage.