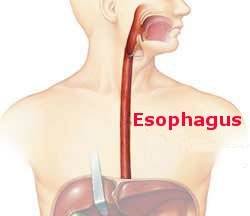
Into the chest.
The chest is the home of most of the esophagus, so it is the location of most cancers. Operating in the chest was impossible until sufficient anesthesia capabilities were established and the lungs could be ventilated. No awake and sentient patient could tolerate the pain of a thoracotomy and it’s impossible to breathe on your own with a chest open to the air.
After the failures of 1902 (please see my previous blog) and subsequent unsuccessful attempts at esophagectomy in the early 20th century by Sauerbruch, conditions were right in 1913 when Torek in New York operated on his patient to resect an esophageal cancer in the chest. A thoracotomy provided access to the esophagus and his procedure, an esophagectomy, was a success in that the patient survived and lived for a decade. The safety of operating in the thorax had been established. Likewise for the ability to remove the thoracic esophagus. What was missing was a technique to reestablish continuity of the gastrointestinal tract so the patient could eat normally. Torek connected the esophagus in the neck to the stomach with a rubber tube that lay on the front of the patient’s chest. This clever device allowed her to swallow normally but she subsisted mainly on liquids and had to live with this unsightly arrangement. She did not enjoy a robust post esophagectomy life.
There was more to learn about the technique of esophagectomy, both to make it a safer operation and to enhance its likelihood of being curative. In addition, the ability to reconstruct the continuity of the gastrointestinal tract so patients would enjoy a reasonable quality of life was equally pressing and demanded attention.