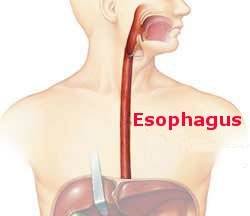
You may never have heard of achalasia. This uncommon disorder of esophageal function was a mystery for many years until physicians took advantage of the advent of esophageal motility studies to first define it and next to develop treatments. Esophageal motility studies use a catheter inside the esophagus to evaluate both the progression of contractions—which should be sequential, i.e., peristaltic, from top to bottom—by the esophageal muscle and the relaxation characteristics of the muscular sphincters at the top of the esophagus in the neck and the bottom where the esophagus joins the stomach.
People with achalasia have difficulty swallowing food. They successfully clear their mouth but the food bolus gets stuck in the esophagus rather than pass uneventfully into the stomach. The motility study explains. There is no peristalsis; all contractions are simultaneous. There is not the normal progression of squeezes to advance the swallowed material as, for example, is the case when you put toothpaste on your toothbrush. To make things worse, the sphincter at the bottom of the esophagus has lost its ability to relax so rather than easing up to let food through the sphincter resists its passage. The end result is an esophagus which cannot push food along and encounters resistance from a muscular obstruction—and a patient who can’t get food into their stomach.
The first recorded treatment (for what had to be achalasia) in 1672 was by Thomas Willis who gave a patient a whale rib with a wad of cloth on the end. The patient used this instrument like a sword swallower might and pushed food through his esophagus and into his stomach for several years. More recent treatments included stretching the lower sphincter with by inflating a balloon and cutting the sphincter muscle surgically. Currently two surgical interventions are in use. In one surgeons use a minimally invasive laparoscopic technique to cut the sphincter muscle to decrease its resistance to food passage. For the alternative approach the surgeon passes an endoscope into the esophagus, penetrates the lining of the esophagus, the mucosa, and then cuts the esophageal muscle. In my opinion the minimally invasive technique is more likely to provide long-term relief but the endoscopic approach has the benefit of not requiring a skin incision.